RESEARCH, EDUCATION & MEDICINE
//
F R O M T H E M E D I C A L L I N E
56
|
FALL 2014
Q:
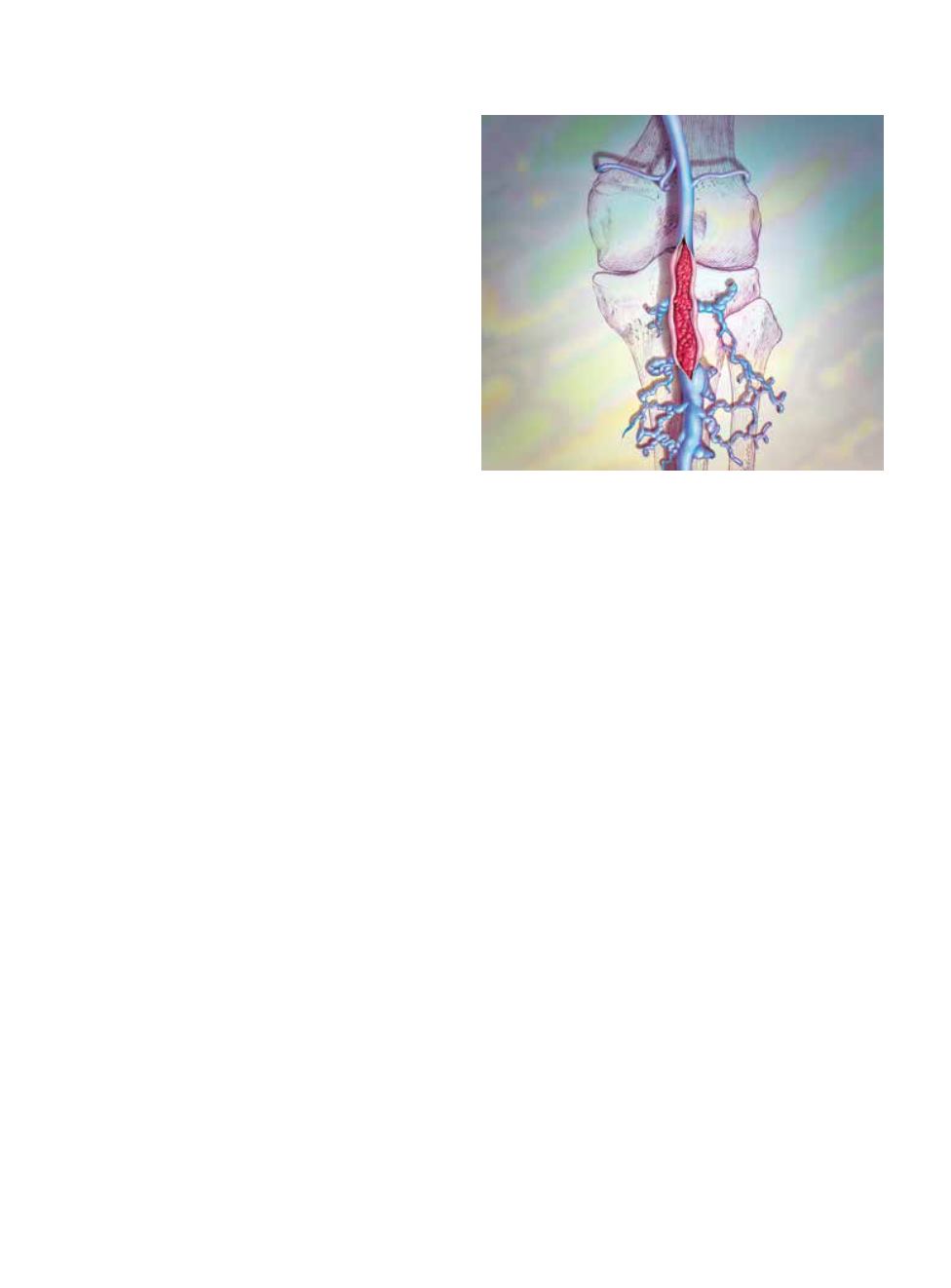
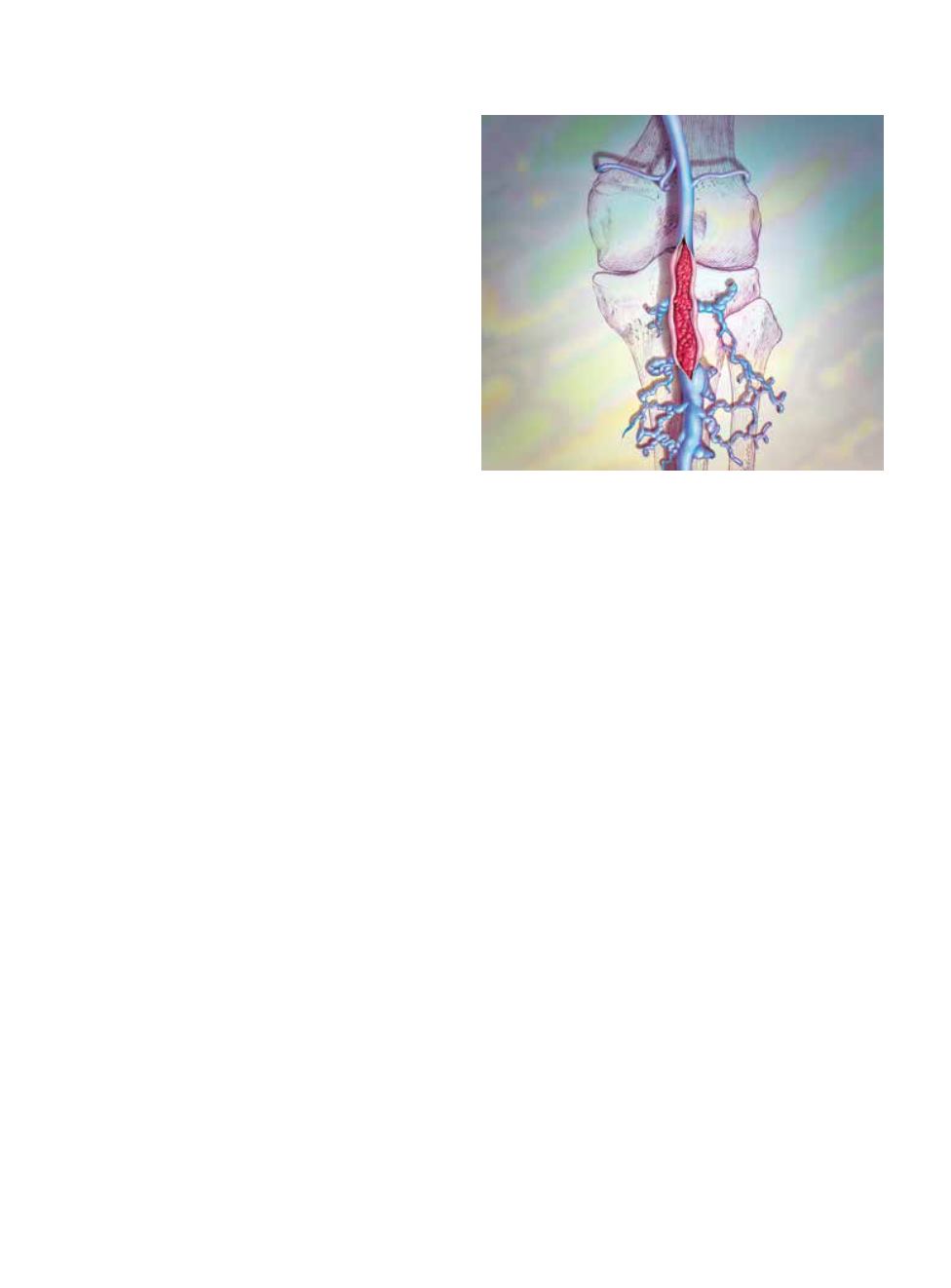
I’ve heard that deep vein thrombosis (DVT) is
a concern for travelers on long flights. What
are the risk factors for getting DVT, and will I
still be able to dive if I do?
A:
DVT is a condition in which a blood clot forms
in one or more of the deep veins, usually in the
legs. When blood clots break free and travel with
the blood, DVT can cause life-threatening conditions such
as stroke or pulmonary embolism. DVT is not related to
diving, but divers often travel and are thus exposed to the
risk of DVT.
Although DVT while traveling is rare (the prevalence
for travelers on flights of more than eight hours is between
0.3 and 0.5 percent), risk factors include older age (with
increasing risk after age 40), obesity, estrogen use, recent or
current pregnancy, thrombophilia, prior personal or family
histories of DVT, active cancer, serious illness, recent
surgery, limited mobility, central venous catheterization
and significantly above- or below-average height.
If you will be on a long flight and believe you might be
at increased risk for DVT, you can reduce the likelihood
of developing the condition by wearing compression socks
and talking with your primary-care physician regarding
the possible benefits of anti-inflammatory medications.
It is also good practice to periodically stand up and walk
around, exercise the feet and calves while you are seated
and stay well-hydrated.
If you develop DVT, you should not dive during the
acute phase of the condition or while you are taking
anticoagulants. You may return to diving after DVT, but
you should not do so before consulting a physician trained
in dive medicine. It is less likely that you will be able to
return to diving after pulmonary embolism, but you may
be able to do so in consultation with a physician. Returning
to diving after a stroke should also be evaluated on an
individual basis.
For more information about DVT, see DAN’s “The Dive
Lab” blog at DAN.org/TheDiveLab/DVT.
— Petar Denoble, M.D., D.Sc.
Q:
I recently went on a dive trip in which the
staff insisted that we should all drink five to
six liters (about 1.5 gallons) of water on dive
days. Is this really a good idea?
A:
This practice is not universal and not
recommended. It is a natural human tendency to
rationalize that if a small amount of something
is good then a larger amount must be better, but that
rationale seldom holds true. Consuming that much water
could actually lead to serious medical problems.
One potential complication is “water intoxication,”
a phenomenon in which excessive consumption of
water leads to a decreased amount of sodium and other
electrolytes outside of the body’s cells. The reduced
sodium concentration outside the cells means the sodium
levels within cells are relatively higher. Water will enter
the cells to try to equilibrate the sodium levels, which
causes them to swell. This in turn can cause skeletal
and abdominal muscle cramping. Furthermore, swelling
in the brain cells can result in confusion, personality
changes, coordination problems and a lack of situational
awareness. Severe, untreated cases of water intoxication
can lead to coma and death.
Another potential complication for divers is an increase
in the fluid volume of the blood. When we are submerged
in water there is a shift in blood volume from the peripheral
vessels to the central circulation. This is expected and
normal. Typically when this blood shift occurs the heart’s
Deep Vein
Thrombosis
and Diving
DAN medics and researchers
answer your questions about
dive medicine.
BODELL COMMUNICATIONS/PHOTOTAKE