She spoke with the resort manager, who transported her to
the local clinic.
As the clinic staff began their evaluation, the first priority
was to empty the diver’s bladder, and they promptly did so
using a urinary catheter. The staff recognized the possibility
of a decompression injury and began making arrangements
with the local hyperbaric facility. They also placed the diver
on high-flow oxygen (15 liters per minute via a nonrebreather
mask). Due to staffing issues the diver was not transferred
to the hyperbaric facility for another two hours, but she did
continue breathing high-flow oxygen during her time at the
clinic and during transport, which was uneventful.
The Evaluation
Upon arrival at the chamber facility the diver was fully alert
and oriented and able to provide the treating doctor with
a detailed account of the events and the evolution of her
symptoms. The physician conducted a neurological exam and
discovered no problems with the diver’s right arm. Strength in
her arms was equal, and reflexes were normal. The soreness
in her middle and upper back had not returned.
Neurological evaluation of the lower extremities revealed
reduced strength in the right hip-flexor muscles compared
with the same muscles on the left side. There was also
reduced sensation in the left leg and patchy areas of altered
sensation in the right leg. Perception of hot and cold stimuli
was altered in both feet. The diver was unsteady while
attempting to walk heel to toe, she found it difficult to stand
on one leg, and she reported that her legs still felt rubbery.
The treating physician diagnosed her with decompression
sickness (DCS) Type II with spinal cord involvement.
The staff initiated a U.S. Navy Treatment Table 6 (TT6).
About halfway through the treatment the diver reported
improvement. Following the treatment, a repeat neurological
evaluation revealed marginally improved strength in the right
leg. The diver also reported improved sensation in her feet.
She was helped back to the resort, where she slept for a few
hours before returning for an additional treatment. During a
shower she noticed improvement in her ability to distinguish
hot and cold sensations. The diver’s ability to walk heel to toe
was also improved, and she had less trouble standing on one
leg. The doctor decided to administer a second TT6, after
which an evaluation showed further improvement.
The next day the diver was evaluated again and treated
with a U.S. Navy TT5 (a shorter chamber treatment), again
with incremental improvement. Three additional shorter
U.S. Navy TT9 treatments were provided. The diver had
reached a clinical plateau, showing no further improvement
after the second and third TT9, so no further treatments
were administered. Some slight sensory decrements were
still present, but the physician’s opinion was that the diver
would continue to improve. After waiting the recommended
72 hours, the diver flew home and experienced no
worsening of her symptoms during the flights. Two weeks
later she reported continued daily improvement with only
mild sensory alteration remaining in her feet.
The Discussion
It would be easy to criticize the boat crew for their failure
to act; they had probably seen people dive those profiles
without incident many times and were thus lulled into
complacency. Further confounding this case was the
spontaneous resolution of most of the diver’s symptoms.
Such resolution of symptoms is typically a response to
breathing oxygen, but in rare cases it may even occur in
the absence of oxygen first aid. Although not all of this
diver’s symptoms resolved, the improvement of most of her
symptoms made this situation appear much less severe than
it actually was.
It is important to remember that the signs and symptoms
this diver exhibited can be considered profound, but even
subtle signs or symptoms warrant at least an informal
conversation to determine the extent of problems. Any loss
of muscular strength should prompt immediate evaluation
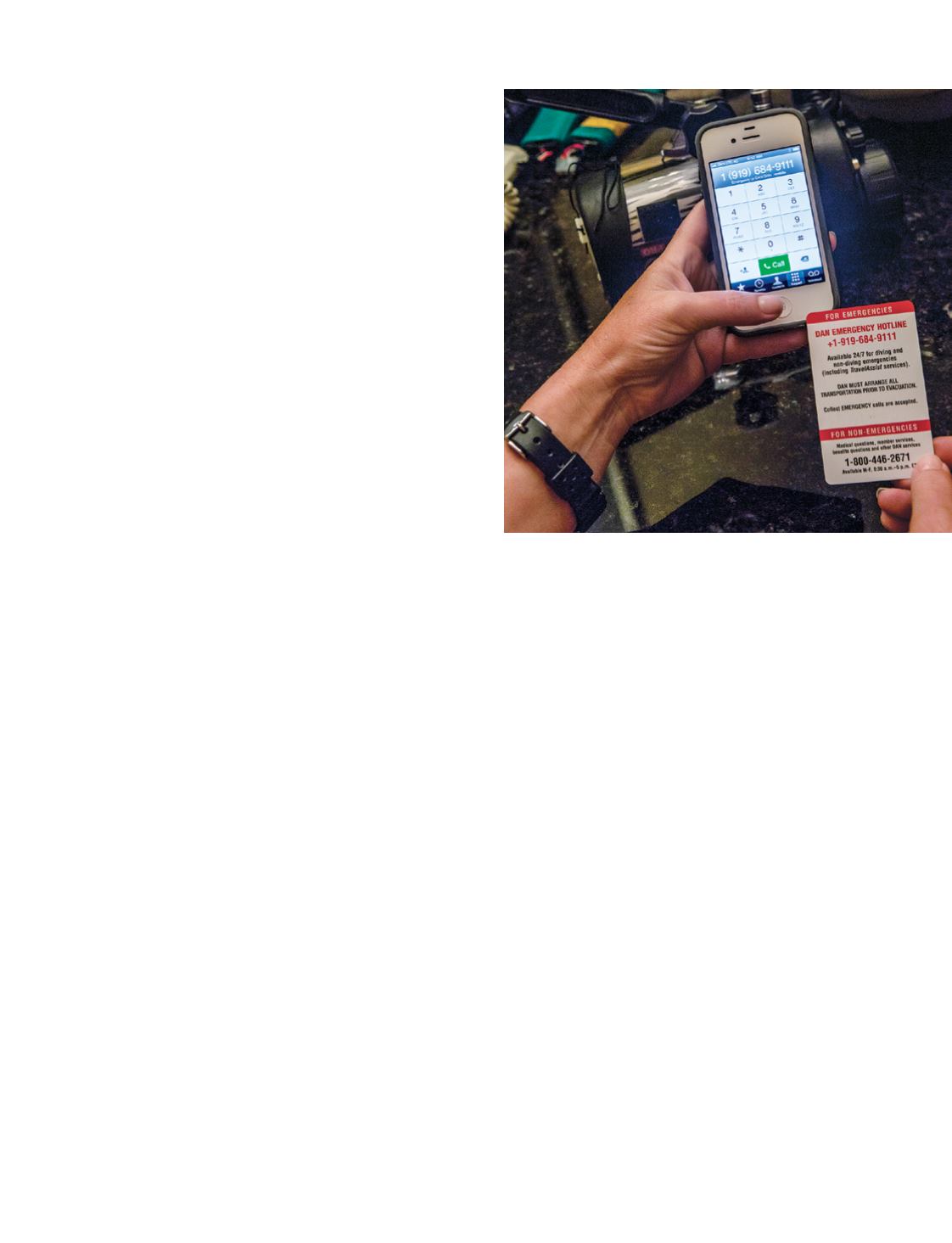
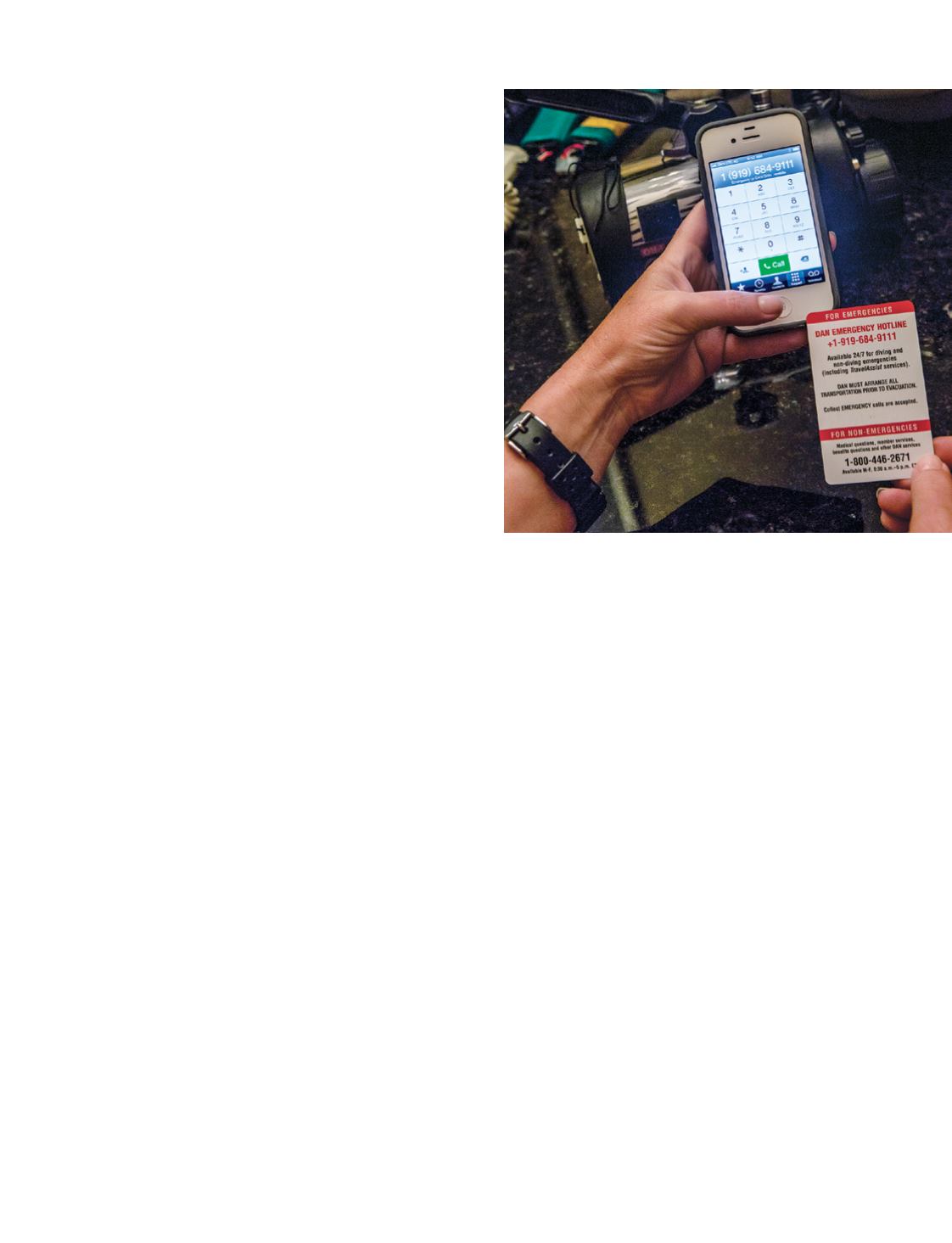
and intervention. The DAN Neurological Assessment course
provides knowledge and skills for recognizing and assessing
potentially injured divers; no matter what training you have,
don’t hesitate to recommend that a diver seek professional
medical evaluation. Regardless of whether symptoms that
appear after a dive are subtle or obvious, if they resolve with
oxygen first aid — or even without it — don’t discount the
possibility that they will return.
AD
|
61
STEPHEN FRINK